Now more than ever, healthcare is an industry in transformation. Heightened government regulation, payment reform, and healthcare consumerism are driving the shift toward new paradigms of care for digital patient engagement. Value-based, outcome-driven models that deliver more personalized, accessible care options are becoming the new normal.
A healthcare industry focused on maximizing value and outcomes will increasingly require organizations across the healthcare ecosystem to work together, improving health data access, fueling innovation, and delivering a more connected and engaging patient experience.
Today’s connected patient demands a more personalized and engaging healthcare experience that offers instant access to health information and services anytime, anywhere, and on any device.
54% of consumers report that they would like to use their smartphone to interact with their healthcare providers1
Facing new patient demands, in addition to Meaningful Use Stage 3 requirements, that provide financial incentives to providers that promote advanced health information exchange to deliver improved outcomes for patients, digital patient engagement has become a key strategic initiative.
Digital patient engagement requires interoperability and wider data access…
Healthcare leaders’ digital patient engagement initiatives are underpinned by the ability to share data across any system and device. But this is easier said than done, particularly within the healthcare industry which has long been plagued by interoperability and data access challenges.
Enter FHIR® (Fast Healthcare Interoperability Resources), an HL7 standard that simplifies the exchange of healthcare information and promotes the use of APIs to support light-weight integration.
Securely exposing and managing FHIR® APIs, facilitates data access and interoperability across the healthcare ecosystem — accelerating time to market for game-changing digital services and experiences that promote deeper patient engagement and improved health outcomes.
By fueling widespread data exchange, API-powered, FHIR®-enabled solutions could enable stakeholders across the patient’s ecosystem to redefine the value and quality of the patient experience by inviting better collaboration and open innovation resulting in a more orchestrated and cohesive healthcare customer experience network.
Today’s patient experience is highly fragmented…
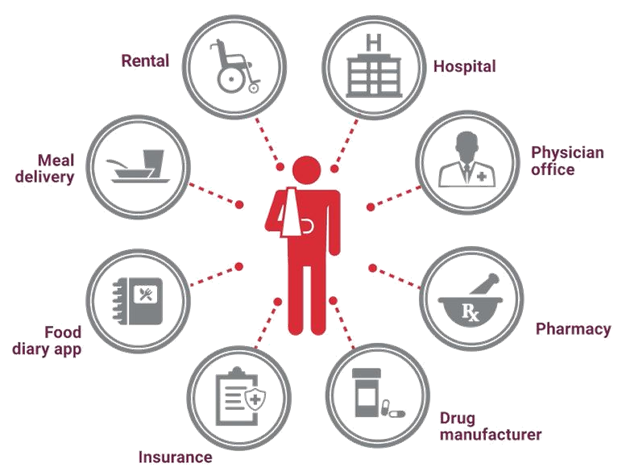
A patient’s ecosystem may include a variety of different, unaffiliated organizations such as hospitals, physician’s offices, pharmacies, health insurance companies, drug manufacturers, and federal agencies.
As a patient interacts with different stakeholders within this ecosystem, their experience is highly fragmented and inconsistent. Data does not seamlessly flow across this ecosystem and as a result, there is no unified, real-time view of the patient.
However, with the support of EHR vendors, and a growing community of developers building FHIR®-enabled software and applications that advance interoperability and broader health information exchange – the way has been paved for a variety of data-intensive initiatives that support patient engagement and population health management across the ecosystem.
The adoption of FHIR® in support of innovative patient services extends to Federal healthcare agencies as well. A key example is the “Blue Button on FHIR®” effort led by the Centers for Medicare and Medicaid Services and the Veteran’s Administration to enable Medicare beneficiaries to connect patient claims data to apps, services, and research programs they trust.
Imagine the possibilities
Patient medication non-adherence costs the U.S. healthcare system upwards of $300B per year.2 Without a unified, real-time view of the patient as they engage with different stakeholders across the ecosystem, it is difficult for a treating physician to get insights into all the medications that have been prescribed and filled by the patient, or administered to the patient by other providers they encounter during the course of care.
Because FHIR® resources cover a variety of clinical and non-clinical elements (e.g., medications, diagnostics, care plans, billing, etc.) and are suitable for a wide variety of contexts (from mobile apps, cloud communications, EHR-based data sharing, server communication in large healthcare systems, and much more) they help enable a more unified view of the patient for stakeholders across the ecosystem.
For example, physicians can identify gaps in adherence (prescriptions not filled or administered) or overfill indicators (duplicate Rx orders or insurance claims) based on improved access to real-time data from other hospitals, physician’s offices, and pharmacies that form part of that patient’s ecosystem.
This provides the opportunity for improved physician-patient engagement and targeted, early interventions that can reduce hospital readmissions, need for emergency care, and ultimately improve outcomes.
Extending this level of data access to drug manufacturers, personal genomics companies, and research institutions provides an opportunity for chronically ill patients to be easily matched to relevant clinical trials or with new precision medicine treatments designed to optimize efficiency or therapeutic benefit for particular groups of patients, using genetic or molecular profiling data, improving access to more personalized treatment options for the patient.
As the adoption of APIs and FHIR® heats up across the industry, patient engagement initiatives will incorporate more data sources and stakeholders resulting in a more personalized and connected patient experience that drives higher quality, more consistent outcomes.
With Axway Amplify, Axway’s market-leading data integration, and engagement platform, health IT leaders can master the full API lifecycle to accelerate digital innovation and meet patient demands for new API-powered apps and services.
Learn more about Axway’s solutions for digital health here.
1HIMSS 2016 Connected Health Survey
2The Express Scripts 2013 Drug Trend Report

